In a groundbreaking development that could redefine cancer treatment strategies, researchers are exploring the concept of putting metastatic cancer cells into a permanent state of dormancy using bioengineered "cages" made from advanced biomaterials. This approach, often referred to as the "dormancy cage" strategy, represents a paradigm shift from traditional therapies that aim to kill cancer cells outright.
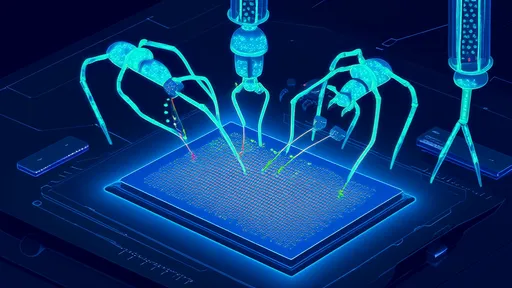
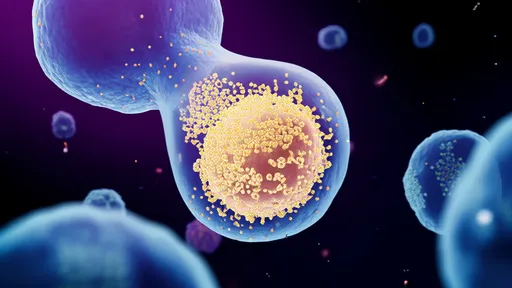
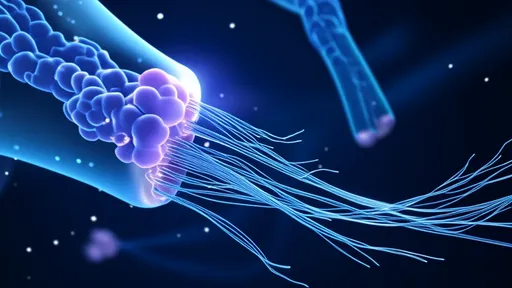
The fundamental premise revolves around creating physical barriers around micrometastases—those elusive clusters of cancer cells that break away from primary tumors and colonize distant organs. Rather than chasing these migratory cells with toxic drugs or radiation, scientists are developing implantable biomaterial scaffolds designed to entrap and biologically isolate them indefinitely. These synthetic microenvironments exploit cancer cells' natural tendency to become dormant when deprived of specific growth signals.
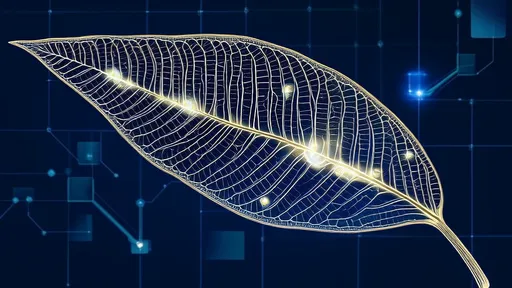
At the core of this technology are sophisticated hydrogel composites that mimic the mechanical and biochemical properties of human tissues. When surgically placed at common metastatic sites like the lungs, liver, or bones, these materials create what researchers describe as an "artificial niche"—a carefully engineered space that tricks disseminated tumor cells into maintaining a quiescent state. The hydrogels contain precisely calibrated stiffness gradients and molecular cues that essentially fool cancer cells into believing they're in an inhospitable environment unsuitable for proliferation.
What makes this approach particularly revolutionary is its departure from conventional cytotoxic methods. Current treatments often inadvertently promote metastasis by creating selective pressure that favors more aggressive cancer cell variants. The dormancy strategy, conversely, neutralizes the threat without triggering evolutionary resistance mechanisms. Early animal studies demonstrate that entrapped cancer cells can remain viable but non-dividing for extended periods—in some cases exceeding the natural lifespan of the host organism.
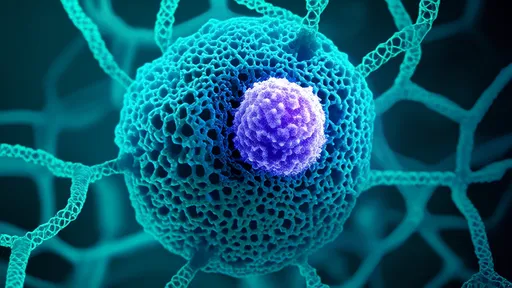
The biomaterials employed in these systems incorporate several ingenious design features. Some versions contain nanopores small enough to allow nutrient diffusion for basic cellular survival but too narrow to permit angiogenesis—the formation of new blood vessels that tumors need to grow beyond microscopic sizes. Others integrate controlled-release systems that deliver microenvironment-modifying agents like tumor-selective cytokines or extracellular matrix components known to maintain dormancy.
Clinical translation faces significant but surmountable challenges. Precise targeting of micrometastases requires improved imaging technologies, and the long-term stability of these implants must be guaranteed. However, the potential benefits are enormous. Unlike systemic therapies that cause widespread collateral damage, localized dormancy induction could dramatically reduce treatment side effects while converting metastatic cancer into a chronically managed condition rather than a terminal diagnosis.
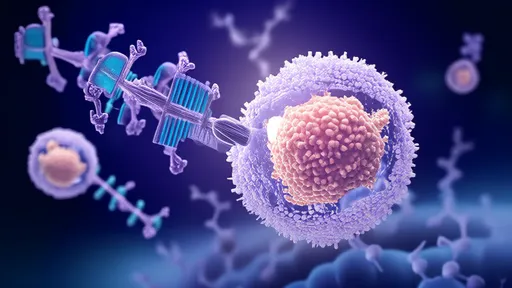
Several research consortia are now advancing toward human trials with optimized versions of these platforms. One particularly promising iteration combines the physical confinement approach with immunomodulatory elements—slow-releasing compounds that keep the immune system vigilant against any cells attempting to escape dormancy. This dual-mechanism design addresses a critical concern about potential late-stage reactivation of contained tumors.
The philosophical implications of this therapeutic strategy are profound. By acknowledging that complete eradication of all cancer cells may be biologically unrealistic in many cases, researchers are pioneering an alternative framework focused on coexistence through control. This mirrors broader trends in precision medicine that emphasize quality-of-life preservation alongside disease management.
As the technology matures, experts anticipate combination therapies where dormancy cages work synergistically with other treatments. Primary tumors might be surgically removed or irradiated while disseminated cells are contained physically. Such integrated approaches could finally provide solutions for aggressive cancers that currently have dismal survival rates once metastasis occurs.
While much work remains, the dormancy cage concept has injected new optimism into metastatic cancer research. By viewing metastasis through an ecological lens—focusing on altering the environment rather than just attacking the invaders—scientists may have found a way to turn one of oncology's most intractable problems into a manageable condition. The coming decade will reveal whether this biomaterials-based strategy can fulfill its transformative potential in clinical practice.
By /Jul 29, 2025
By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025
By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025
By /Jul 29, 2025

By /Jul 29, 2025
By /Jul 29, 2025

By /Jul 29, 2025
By /Jul 29, 2025
By /Jul 29, 2025
By /Jul 29, 2025
By /Jul 29, 2025

By /Jul 29, 2025
By /Jul 29, 2025
By /Jul 29, 2025